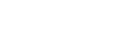
Photograph by Audra Melton
Like so many patients who find their way to the HEALing Community Center in Southwest Atlanta, Robin Swinks came with a sense of desperation. She needed a doctor who would listen to her story—someone to help her forge a way through the healthcare labyrinth.
So on a Wednesday evening, she sat on an exam table while clinic founder Dr. Charles Moore gently felt her nose and peered inside her nostrils. About three months earlier, Swinks, 37, had been in a serious car accident that left her with a severe concussion, memory loss, and a shattered nose. The headaches subsided, the memory came back, but so far the insurance company had refused to fix her nose.
“They make it seem like I’m a bored housewife who does not like my nose,” she said, her voice high-pitched and strained. “I have made it clear that I cannot breathe.”
Moore, an ear, nose, and throat doctor, nodded. Swinks’s nose had shifted to one side, and fractures had left a hump and S-shaped crook. Inside, the septum, which separates the nostrils, had been crushed. It was blocking one nostril by about 80 percent and the other by 50 percent.
“That should ultimately be approved by your insurance,” he assured her. “I’ll get several folks involved to help clear it and get it done.”
There was no bill or co-pay for the exam, just some instructions about how to register at Grady Memorial Hospital before he met with her again. Moore specializes in surgery for craniomaxillofacial trauma and anterior cranial base tumors—and in helping people overlooked by the healthcare system.
“I love the mission of this place. It’s great work they’re doing,” Swinks said as she left. “His whole mission is speaking for people who aren’t spoken for.”
A quiet man lacking even the slightest swagger of an Ivy League–educated physician, Moore never set out to save the world. He wasn’t thinking about underserved populations when he left his home state of New York for Harvard Medical School and then specialty training at the University of Michigan—eventually becoming an associate professor at Emory University and chief of otolaryngology/head and neck surgery at Grady Memorial Hospital.
But Moore had never experienced what he saw at Grady. Patients with big, bulbous tumors on their tongues. Patients with tumors the size of tennis balls in their necks. Patients who were the walking dead because it was too late to save their lives.
When Moore asked them why they hadn’t sought care sooner, he heard common refrains. With little money, they chose buying food over medicine. They didn’t have insurance. They didn’t have transportation. “Somebody needs to do something about this,” Moore thought to himself with a sense of outrage whenever he saw an advanced cancer that could have been treated if caught earlier. Then one day, Moore realized, “Maybe that someone should be me.”
It wasn’t hard to figure out where these patients were coming from. Moore studied their charts and saw the zip codes 30314, 30318, 30311—neighborhoods due west, where one in three people live in poverty, the unemployment rate is 19 percent, and nearly one in four people have no health insurance.
These neighborhoods are a case study of health disparity, an enclave where people are more likely to die early of stroke, cancer, and diabetes than their counterparts across the county in Roswell or Johns Creek. These are places where residents struggle just to get to and from a grocery store, let alone across town to see a medical specialist.
Moore drove past this area every day, a blur of drab concrete and kudzu, as he zipped along Interstate 20 on his way home to Mableton. But one day, he decided to take a closer look. He shed his necktie, loosened his collar, and took an exit ramp that led to Donald Lee Hollowell Parkway. (It was then called Bankhead Highway, a name immortalized by rappers and erased by city leaders embarrassed by its high crime rate.) He drove past overgrown lots and cinder block buildings with bars on the windows, houses that needed repair and chain link fences topped with barbed wire. He saw an older woman waiting for a bus, so he parked nearby and approached her. He didn’t mention that he was a doctor. He just struck up a conversation about the community.
“I didn’t get her name; she didn’t get mine,” he says. “As I recall, she was headed to work and it was in the late afternoon. The day before, someone had been shot. We started talking about that, and she talked about how raising her kids, she was always concerned something was going to happen to them.”
Moore didn’t really know what he was going to do, but he kept detouring off the highway. He kept talking to people. “It was just a personal venture more than as an M.D.,” he says.
Can one man make a difference? That question dogged Moore in his trips along Hollowell Parkway, Hamilton E. Holmes Drive, Martin Luther King Jr. Drive—streets named after icons of the civil rights movement that traversed some of the bleakest spots in metro Atlanta.
An answer settled on him. He thought to himself, “Sometimes it’s not the magnitude of what you do. It’s the fact that you’re doing something to make a difference, and people sense and feel that.”
Moore got a big Tupperware container and filled it with tongue depressors, gauze, gloves, alcohol wipes, and disposable dental mirrors to look into the throat. He drove to churches and homeless shelters and health fairs, offering head and neck screenings. His green Subaru Forester (which now has almost 300,000 miles) became a familiar sight, a roving doctor’s clinic that needed no fancy logo.
These were people who never received medical care, so Moore had to brush up on his primary care skills and tend to basic needs. Once, someone asked him to go to a crack house. He hesitated, but ultimately decided his goal was to reach the unreachable, so he agreed. (He never saw any illegal activity while he was there.)
“I remember one guy in particular,” says Moore. He had a small cancer on the side of his tongue, but he lived about 10 miles from Grady. “I was so concerned about how he was going to get to Grady [for surgery]. He said, ‘Don’t worry about it. No one has ever shown us any kind of concern. I’ll get there.’”
The man walked. And arrived early for his appointment.
Perhaps more than anything, that man’s persistence defined for Moore the daily barriers faced by these residents and their pent-up desire for care.
Soon other clinicians expressed interest in donating their time. “Most folks who go into medicine really do just want to help people,” he says. “It reignited something in them about why they went to medical school or nursing school or other health-related fields.”
So eight years ago, he founded HEAL (Health Education, Assessment & Leadership) and applied for a grant from Mobile Medical Ministries International, a faith-based nonprofit that supports mobile medical clinics for underserved communities. He obtained a mobile unit and called it the HEALing Community Center.
Moore has since learned the power of collaboration, finding clinic space first with a community service organization, then in a vacated Grady clinic. About 45 percent of the patients are unemployed or disabled, and more than 80 percent are uninsured. In a recent survey, 40 percent of patients said they would have gone to an emergency room if the center had not been available; about the same number said they didn’t know where they would have gone.
In 2011, Moore began working with Emory University’s Urban Health Initiative and became its codirector, which opened new opportunities. The initiative was founded by Emory neonatologist William Sexson, who thought there should be a local counterpart to the university’s Global Health Institute, which supports research and training on public health problems around the world. Teams of Emory undergrads and public health, medicine, nursing, and business students have now signed on to address human suffering just across town.
The initiative shares Moore’s philosophy of asking people in the community what they need. “We assume we do not know much about their situation,” says associate director Carolyn Aidman. “We learn from them, and we try to help them come up with solutions that will make a difference.”
For example, the Bankhead area is a “food desert,” where grocery stores are scarce and it’s hard to get fresh, healthy, and affordable food. With funding from the Coca-Cola Foundation and the Woodard & Curran Foundation, the Urban Health Initiative created a community garden in the parking lot of a Super Giant Food grocery store on Hollowell Parkway.
Emory students also spent hours labeling shelves at the Super Giant and a nearby Walmart with tags highlighting the healthiest choices, a project of Food Oasis, a coalition of 13 Atlanta organizations that promotes better nutrition. The Super Giant is even creating space for a satellite clinic of the HEALing Community Center.
But how do low-income residents get to and from the grocery store and laundromat, with bags and children in tow? They pay $30 to the “Ride Man”—who will wait 30 minutes, but then might get impatient and leave riders stranded, Aidman discovered. How do pregnant women get to Grady to have a baby? They call 911 for an ambulance because they can’t stand outside in full labor, waiting for a MARTA bus.
Using a neighborhood church bus, the Urban Health Initiative is creating a simple loop on Wednesdays from the largest subsidized-rent apartment complex to the laundry, grocery store, children’s schools, and the clinic. Another idea in the works is having an Uber driver transport women in labor, a project dubbed “the Labor Limo.”
Meanwhile, the HEALing Community Center continues to expand. It has a staff of 20, providing primary care, pediatrics, and even dentistry. Cardiologists from Piedmont Hospital volunteer twice a month, and HEALing patients needing cardiac procedures can get free treatment at Piedmont. Other free specialty care includes pulmonology, ophthalmology, obstetrics and gynecology, mental health services, and audiology. Students from Morehouse School of Medicine help with community needs assessment.
As a federally qualified health center, the clinic receives increased reimbursement from Medicare and Medicaid to support ongoing expenses. And nutritionists and chefs provide health education along with Fulton Fresh, a healthy foods project of the Fulton County Cooperative Extension Service. The Atlanta Falcons Youth Foundation sponsors the Food Oasis and Fulton Fresh projects.
Promoting a healthy lifestyle is an important part of Moore’s mission. He started with “prescriptions” for health: “Kale, Monday-Wednesday-Friday” or “Walk 3 times a week for 30 minutes” scrawled on a prescription slip. He put pictures of fruits and vegetables on doors so they could send someone to the “apple room” instead of exam room four. Once a month, he mixes exercise with health education in his “Walk with a Doc” hikes at Lionel Hampton-Beecher Nature Preserve.
And Moore continues to reach for new connections. For example, the HEALing Community Center provides healthcare for children in a nearby church daycare. “Otherwise, the parents would not be able to access those services,” says the Reverend Larry Hill, pastor of the Word of God Ministries. “These are the kind of partnerships that really make a great impact.”
On a stormy fall morning, Lavern and Bonita Evans venture from their home in College Park for an appointment at the HEALing Community Center. Lavern, 62, started feeling the achiness and tightness in his joints hours before the first rain fell, and when he rises from a chair in the waiting area to help his wife, he feels razor-like pain in his knee and hip and steadies himself with a metal cane. Bonita, 59, is legally blind, able to see only through a pinhole in her left eye and not at all in her right eye, due to untreated glaucoma.
And yet Lavern is smiling. They are doing much better than they were when they first arrived at this clinic a couple of years ago. Lavern was suffering from depression and pain from a work accident that had fractured two vertebrae in his neck, damaged joints and muscles on his right side, and caused a severe concussion. After spending most of his days in bed, he weighed almost 400 pounds.
Bonita, a diabetic, was bumping into furniture but thought she just needed a new eyeglass prescription. Without health insurance or a referral from a doctor, she couldn’t get an appointment to see an ophthalmologist, even at Grady.
“This is the only place in the six and a half years I’ve been down that didn’t close the doors on me,” says Lavern.
A family medicine physician at the clinic helped them get into the Grady system, where they were able to qualify for Medicaid. The Evanses also started attending health education classes at the HEALing Community Center, where a nutritionist taught them how to shop for healthy food and how to prepare it—starting with a bag of free vegetables.
They swapped fried chicken for grilled or baked; added kale, squash, and other vegetables to their diet; and cut out fast food. Lavern has lost 60 pounds so far. Bonita’s diabetes is under control. Lavern plans to visit the new dental clinic to address problems caused by the teeth he lost in his accident. “Without this, we’d probably still be beating our heads against the wall, trying to get help,” he says. “It’s a lifesaver to me. It was a game changer, completely.”
This article originally appeared in our 2015 Health issue.