Photograph by Ben Rollins
ACCESS TO HEALTHCARE
Jermaine Jackson, MD
Pulmonologist and critical care specialist
Piedmont Healthcare
Director
Piedmont Pulmonary Covid-19 Recovery Clinic
Around July of 2020, we started exploring what happens to [Covid] patients once they are out of the hospital. That was the genesis for what we have now termed a Covid recovery clinic. At that time, the nomenclature of “long-hauler syndrome” was not in existence—we did not know that was something that would happen.
In November 2020, we opened the doors of our Covid recovery clinic. The purpose was to deal with both the recovery and the long-hauler phase for those who have prolonged or protracted symptoms, typically defined as about 12 weeks after infection. So far, we’ve had right at about 1,400 referrals to our clinic.
The pandemic has exposed some things related to the delivery of healthcare services. We have to recognize that, globally, there is an inadequate healthcare workforce. There are not enough physicians, nurses, allied health professionals, and other ancillary services. The entire system is woefully understaffed. We’re going to have to enhance our pandemic preparedness.
It also exposed healthcare inequities. Social disparities impacted all of healthcare, including the death toll.
And a third thing is understanding the need for collaboration across communities, across counties, across countries—global collaboration. We’re going to have to remove barriers so we can leverage technologies and [share] information and electronic medical records.
Dealing with inequities begins with, number one, obviously acknowledging the fact that we have disparities. Part of that is because of the cost of healthcare. I’m not necessarily pushing for so-called socialized medicine, but I do believe that healthcare is a right—a right to basic care and preventative services.
Also, we don’t often talk about the social determinants of health. These are the things outside the walls of the healthcare system—transportation access, food deserts and lack of food security, and [exposure of] frontline workers such as bus drivers, grocery-store workers, etc. You start with some of the very basic things that are important just for life itself—food, water, clothing, shelter—and try to deliver support in those areas. Here in the United States, we’re so blessed to have a lot of resources, but unfortunately, those resources are either withheld or not deployed to the vulnerable people most in need. The pandemic has helped, once again, highlight things that we historically have known. We were able to put numbers to it when we saw the death tolls among certain populations.

Photograph by Ben Rollins
PREVENTIVE HEALTHCARE
Mindy Gentry, MD
Cardiologist
Wellstar Health System
From a physician’s perspective, our goal is to prevent things from happening rather than coming in after the fact. It’s the plain old boring stuff: diet, exercise, good nutrition, not smoking, just taking good care of yourself. I do think the pandemic has made people more aware of their underlying health. People have been paying attention to risk factors that tend to make you have problems or complications related to Covid, things like underlying heart disease and obesity. People have a renewed sense of the importance of controlling those risk factors.
During the pandemic, people have taken one of two pathways. Many people were less active, scared to get out and do anything, and did gain a lot of weight. They were at home, they were snacking, not eating quite as well. Then, you had another set of people who took advantage of working from home and were able to increase their exercise and actually seemed to be in better shape—but that’s probably a relatively small minority.
As people are getting vaccinated and community transmission is getting lower, people are more comfortable getting back to the gym or even just getting out and going for walks in their neighborhood. A lot of people are starting to say, Okay, I’ve gained this weight. I haven’t been exercising. I’ve got to get back to it.
Also, the global-health crisis created a new normal that included mandatory quarantines, social distancing, and mask-wearing and brought a new appreciation for the medical and scientific community, which worked tirelessly to develop new medications and vaccines to defeat the deadly coronavirus. There’s been an increased appreciation for our industry peers who specialize in basic, fundamental science—who developed the vaccines in an incredibly rapid time frame. They never get any attention.
And patients have been saying to me, Be safe, be careful. Thank you for being here to take care of me. That means as much or more than anything else.

Photograph by Ben Rollins
CLEAR COMMUNICATION
Brian Vickery, MD
Director, Children’s Food Allergy Program
Children’s Healthcare of Atlanta
The emergence of SARS-CoV-2 led to the first global pandemic to occur in the internet age. What occurred—and is still occurring—is not only an infectious-disease pandemic but also an infodemic. Unfortunately, we have learned that it is challenging to communicate complex and evolving medical and scientific information to the public in an era when everyone has access to a diverse ecosystem of news, opinion, social media, and other forms of communication. When the control of an infectious disease largely depends on collective behaviors, it is critical that people understand what they are supposed to do and why. The amount of information that can be accessed is nearly overwhelming, and in this kind of media environment, we have seen how easy it can be for the public to become confused or skeptical. We have even seen disinformation and the promotion of false or unproven methods in the prevention and treatment of Covid-19.
The CDC’s reversal on whether or not to wear a mask at the beginning was one of the key events that caused people to develop a sense of mistrust. That was unfortunate. At the time, we really did think that Covid was spread by droplets, not aerosol, and there were concerns about availability of PPE for frontline workers.
When scientists change their minds, it doesn’t mean they don’t know what they’re talking about. It means they have more data and a better understanding. That’s the way science works. Science is a self-correcting enterprise.
It will not be easy to put this genie back in the bottle, but we must strive to promote scientific literacy and improve our methods of communication around critical topics such as public health. We need to include media literacy in education and help people learn to separate facts from opinions.
On the positive side, the flow of information also allowed vaccines to be developed in record time. The genetic sequence of this virus was shared globally before it even had a name. Scientists were able to share their findings through preprint servers without waiting for peer review. The rapid breakthroughs that have now begun bringing this virus under control in some countries will be remembered in history as a monumental human achievement, on par with the Apollo moon missions.
Photograph by Ben Rollins
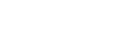
TELEMEDICINE
Joon Ahn, MD
Electrophysiology
The Heart Center of Northeast Georgia Medical Center
Prior to the pandemic, we had talked about setting up a teleconsult service for outlying hospitals in North Georgia, but we’d never officially put anything in place. When the pandemic hit, we very quickly shut down the outpatient clinic and converted patients to televisits to ensure they were seen and had access to care. It was kind of a frenzied time—not just for us but for health systems across the country. We were scrambling to use what technology and resources we had—FaceTime, an app called Doximity, Zoom. We pulled it together extremely quickly. There were a lot of technical issues at the beginning as patients and providers adjusted. Some of our patients had an Apple watch or technology called Kardiamobile, which enabled them to record their EKG and send it to us via text or email. If needed, we were able to send some patients remote monitoring equipment through the mail.
The hospital did an excellent job of helping get patients the care they needed. Eventually, we were able to establish a smooth workflow and a way to connect with patients virtually. It’s actually a pretty seamless process. On the inpatient side, we set up something like a telemedicine cart that a nurse could bring into the room of a Covid-positive patient. We’d be able to interview the patient through an iPad. They’d also have remote electronic stethoscopes that we’d be able to listen to and document heart sounds. This prevented us from having to use excess PPE, which was crucial during shortages. Only the single nurse who would be in the patient’s room would have to wear full gear. This type of technology absolutely could be utilized for consults at outlying hospitals moving forward.
Now, we’ve converted back to more in-person visits, but I think we’ve seen great success with teleconsults and video visits. It will be part of our future.

Photograph by Ben Rollins
MENTAL HEALTH RESOURCES
Toby D. Goldsmith, MD
Assistant Professor, Psychiatry and Behavioral Sciences
Emory University School of Medicine
Director
Emory Women’s Mental Health Program
Founder
PEACE (Perinatal Psychiatry, Education, and Community Engagement) for Moms, which provides support for women’s mental health before and after childbirth throughout Georgia
What I’ve seen over the last 14, 15 months is a need to take care of our own colleagues. There are an increased number of physicians, nurses, and other healthcare workers who’ve said, I’m overwhelmed, I need help. People are finally comfortable with reaching out and saying, I need some assistance. Our department put together a wonderful program so that individuals could talk to a psychiatrist or a psychologist from 6 a.m. until 11 p.m. We had support groups throughout the day. If healthcare workers had said, I can’t be here, the whole system would’ve fallen apart.
Anxiety has exploded. Individuals are afraid of things they weren’t afraid of before. They’re afraid of strangers, especially strangers without masks. And then, there are those who are afraid of strangers with masks. I think we’re going to see a very slow progression back into the real world, the world we were accustomed to prior to March 2020.
This was a very traumatic year for all of us, and it wasn’t just the pandemic. It was also politics and race relations. It just added up. I think people are going to find they are not as resilient as they once were.
I deal with a wide swath of women between 20 and 45. Many, many women put off conceiving because of fear. If they were already pregnant, they had to prepare to enter the system by themselves. They weren’t able to share the experience with their partners, which was extremely difficult. There was a lot of loneliness in a process that should be one of those times you’re surrounded by a village. And then, I saw infighting among families because parents chose to keep their children away—especially if grandma and grandpa weren’t quarantining in a way that would’ve helped.
How will healthcare change? I think we’re going to depend on telehealth. For psychiatry, it works. The advantage is we’ll have the opportunity to treat a lot more people, to give access to patients who never had the ability to see someone. And that’s a blessing.
Photograph by Ben Rollins
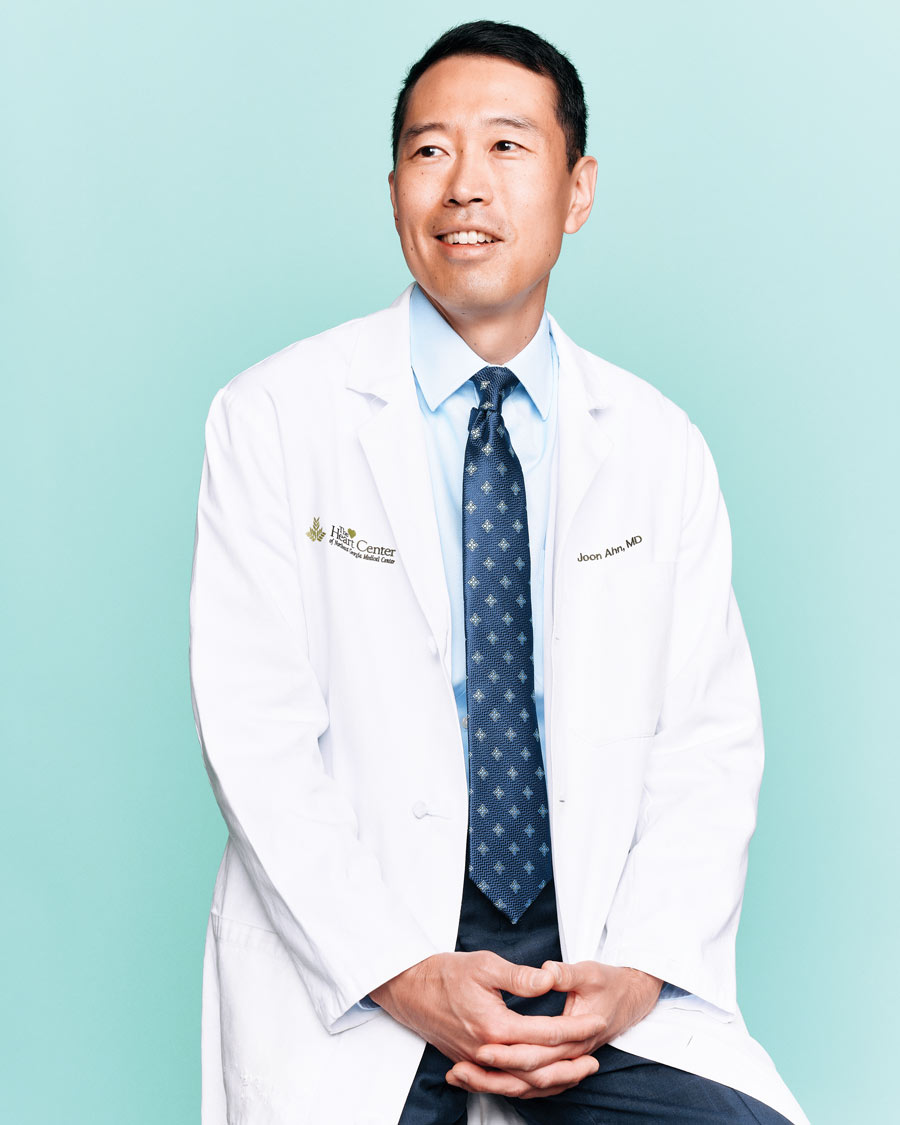
COORDINATED RESOURCES
Bruce S. Ribner, MD, MPH
Professor of Medicine
Emory University School of Medicine
Principal investigator
National Emerging Special Pathogens Training and Education Center
[Editor’s note: also one of the Ebola fighters named TIME magazine’s Person of the Year in 2014]
Emory took care of four patients who were infected with Ebola virus disease. The Department of Health and Human Services then came to us in 2015 and asked us to form a collaboration with the University of Nebraska Medical School and NYC Health and Hospitals/Bellevue. That has evolved into the National Emerging Special Pathogens Training and Education Center. We had a pretty robust program with regional centers all over the country to care for somebody who came to the United States with a serious communicable pathogen. We were pretty comfortable that we could deal with that. But Covid showed us that we had a lot more to do.
The U.S. healthcare system was totally disorganized. We had healthcare systems and states competing to buy personal protective equipment. We would go to a manufacturer and say, We’re running out of N95s. And they would say, Well, we’ve just sold them to New Jersey. We’ve also seen disadvantaged communities suffering disproportionately—proving again that healthcare is not equally provided to all individuals.
How do we have a system that can handle the next outbreak—not if, but when, it occurs? We have impaneled a group of 30 to 40 healthcare experts from around the United States, and we’re in the process of developing what we now have called the National Special Pathogens System. Our goal is to have a truly coordinated system, in terms of medical resources. We especially need access for hospitals and healthcare facilities in underprivileged areas because we’ve clearly recognized they’re underfunded. Our goal is to have a proposal by July. We envision it would take anywhere from three to five years to really have something like this as functional as we would like it to be.
We’re working out the funding. One thing we have learned over the years is that if you depend only on federal government funding, you’ll be on a roller-coaster ride. There are years like 2009 when swine flu hit and they gave us all sorts of resources. There were other years when people would say, Well, there’s no outbreak this year, so why do you need any resources? If you’re really into the job of preparedness and making sure you’re operational when the next event occurs, you need much more robust financing. We are working with private payers, with insurance companies, and with a whole host of different entities to develop a self-sustaining program.
There will certainly be another outbreak. The only question is, do you want to be prepared to control it? Or do you want to have a catastrophe as we did over the last year? Aren’t about 500 people still dying every day from Covid-19 in the U.S.? It’s amazing. We’re looking at that and saying, We’ve got control of this outbreak. Suddenly, that’s a victory?
This article appears in the July 2021 issue.